Introduction
Navigating the path to parenthood can be filled with hope, anticipation, and often, questions. For many individuals and couples, Intrauterine Insemination (IUI) offers a promising step forward in their fertility journey.
This common fertility treatment option involves directly placing specially prepared sperm into the uterus around the time of ovulation, aiming to increase the chances of conception.
The Intrauterine Insemination Process isn’t just a single event; it’s a carefully orchestrated sequence of steps, each playing a vital role. Understanding these phases can empower you, providing clarity on what to expect and helping you feel more in control.
We’ll break down the entire IUI treatment into four distinct and essential phases, guiding you through everything from initial preparation to the much-anticipated pregnancy test. This comprehensive guide will explain how intrauterine insemination works, ensuring you’re well-informed as you embark on this significant journey towards expanding your family. https://dorengynaecareivffertility.com/intrauterine-insemination-iui/
Phase 1 of the Intrauterine Insemination Process: Comprehensive Assessment and Preparation
Before any active steps are taken in the Intrauterine Insemination Process, a thorough foundational phase is crucial. This initial period is dedicated to understanding your unique fertility landscape, identifying any underlying factors, and establishing a personalized treatment plan. It’s where your reproductive specialist gathers all the necessary information to optimize your chances of success.
Initial Consultation and Medical History Review
Your journey typically begins with a detailed consultation at a specialized fertility clinic. This appointment is your opportunity to openly discuss your fertility goals, medical history, and any previous attempts at conception. The specialist will ask about menstrual cycles, past pregnancies, surgeries, and any known health conditions for both partners.
It’s a critical step in determining if IUI is the most suitable infertility solution for your specific situation. This phase also helps identify who is a good candidate for IUI, such as individuals or couples facing mild male infertility, unexplained infertility, or those with cervical factor infertility. For single women or same-sex couples, IUI with donor sperm is a common and effective pathway.
Fertility Testing and Diagnosis
Following the initial discussion, a series of targeted fertility tests are conducted. For the female partner, these often include blood tests to assess hormone levels (such as AMH, FSH, LH, and TSH), which provide insights into ovarian reserve and thyroid function.
Ultrasound scans are performed to visualize the ovaries and uterus, checking for any structural issues. In some cases, a hysterosalpingogram (HSG) may be necessary to ensure the fallopian tubes are open. For the male partner, a comprehensive semen analysis is performed to evaluate sperm count, motility (movement), and morphology (shape).
These diagnostic tests are fundamental; they help pinpoint potential challenges and guide your specialist in designing the most effective IUI procedure steps tailored just for you.
Personalized Treatment Plan Development
Based on the results from the extensive testing, your reproductive specialist will develop a personalized treatment plan. This isn’t a one-size-fits-all approach. The plan will outline the specific medications, monitoring schedule, and timing for your IUI treatment.
It’s a collaborative process where your questions are answered, and expectations for the entire Intrauterine Insemination Process are clearly set. Understanding this blueprint upfront helps you feel more prepared and confident as you move into the active phases of your journey towards conception.
Phase 2 of the Intrauterine Insemination Process: Ovarian Stimulation and Cycle Monitoring
Once the initial assessment is complete and a personalized plan is in place, the Intrauterine Insemination Process transitions into its second, highly dynamic phase: ovarian stimulation and precise cycle monitoring. This stage focuses on optimizing the number and quality of eggs released, ensuring the timing for insemination is absolutely perfect.
Ovulation Induction with Fertility Medications
For many undergoing IUI, especially those with irregular ovulation or unexplained infertility, fertility medications are prescribed to stimulate the ovaries. These medications, often referred to as ovulation induction agents, encourage the development of one or more mature follicles—the fluid-filled sacs in the ovaries that contain eggs.
Common medications include oral options like Clomid (Clomiphene Citrate) and Letrozole (Femara), which encourage the body to produce hormones that stimulate follicle growth. In other cases, injectable Gonadotropins (like FSH or HMG) may be used for a more potent stimulation, leading to multiple egg development.
The choice and dosage of medication are meticulously tailored by your specialist based on your individual response and diagnostic results, aiming to produce an optimal number of healthy eggs without excessive stimulation.
Follicular Monitoring (Ultrasounds & Blood Tests)
This is the phase of close observation. Throughout your stimulation cycle, you’ll have frequent appointments at the fertility clinic for follicular monitoring. This typically involves a series of transvaginal ultrasound scans and blood tests.
The ultrasounds allow your specialist to visually track the growth of your ovarian follicles, measuring their size and counting their number. Simultaneously, blood tests measure key hormone levels, particularly estradiol, which rises as follicles mature, and progesterone, which indicates impending ovulation.
This meticulous ovulation induction monitoring is crucial for identifying the precise timing for the next steps in the Intrauterine Insemination Process. It ensures that the uterine lining is also optimally prepared to receive an embryo, ready for conception with IUI.

The Trigger Shot: Timing Your IUI
Once the monitoring indicates that your follicles have reached an ideal size and your hormone levels are just right, a “trigger shot” is administered. This injection, typically human chorionic gonadotropin (hCG), mimics the natural LH surge that triggers ovulation.
The trigger shot is precisely timed, as ovulation is expected to occur approximately 36 hours after its administration. This allows your specialist to schedule the IUI procedure for the exact moment when the eggs are expected to be released from the ovaries, maximizing the chances of sperm meeting egg and leading to successful conception. This precise timing is paramount in the success of the Intrauterine Insemination Process.
Phase 3 of the Intrauterine Insemination Process: Sperm Preparation and the IUI Procedure
With ovarian stimulation complete and ovulation precisely timed, the Intrauterine Insemination Process moves into its pivotal third phase: the actual preparation of the sperm and the insemination procedure itself. This stage is relatively quick but incredibly precise, focusing on delivering the highest quality sperm to the optimal location.
Sperm Collection and “Washing” Techniques
On the day of your IUI, the male partner will provide a fresh sperm sample, typically collected at the fertility clinic. If donor sperm is being used, a frozen, pre-screened sample will be thawed. Once collected, this sample undergoes a crucial laboratory process known as “sperm washing” or sperm preparation. This technique involves separating the highly motile, healthy sperm from the seminal fluid, non-motile sperm, and other cellular debris.
The seminal fluid, in its natural state, contains prostaglandins and other compounds that can cause uterine cramping if introduced directly into the uterus. The washing process concentrates the best quality sperm into a small, highly concentrated volume.
This careful preparation ensures that only the most viable sperm are used, increasing their chances of reaching and fertilizing an egg, and minimizes discomfort during the IUI procedure. For those undergoing donor sperm IUI, this step ensures the thawed sample is ready for optimal use.
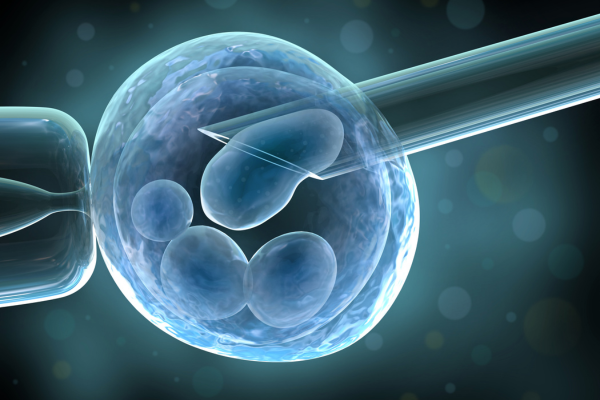
The Intrauterine Insemination Procedure Itself
The Intrauterine Insemination Procedure is a straightforward and generally well-tolerated process, often compared to a routine Pap smear. You’ll lie on an examination table, similar to a gynecological check-up. The specialist will insert a speculum into the vagina to visualize the cervix. A thin, flexible catheter, pre-loaded with the prepared, “washed” sperm sample, is then gently guided through the cervix and directly into the uterus.
The sperm is then slowly injected. This direct delivery bypasses the cervix, which can sometimes act as a barrier to sperm reaching the uterus, thereby increasing the number of sperm available to meet the egg in the fallopian tube. The entire IUI procedure typically takes only 10 to 15 minutes, with the actual insemination taking just a few moments. While some women may experience mild discomfort or a sensation of cramping, it is usually brief and subsides quickly.
Immediate Post-Procedure Care and Expectations
Immediately following the Intrauterine Insemination Process, you’ll typically be asked to lie down for a brief resting period, usually 10-15 minutes, though studies suggest this doesn’t significantly impact success rates.
After this short rest, you can generally resume most of your normal daily activities. It’s common to experience some mild spotting or light cramping for a day or two after the procedure, which is usually not a cause for concern.
Your specialist will provide specific post-IUI instructions, which might include avoiding strenuous activity for a short period. This phase culminates with the sperm now in the uterus, poised for potential fertilization, setting the stage for the next period of anticipation.
Phase 4 of the Intrauterine Insemination Process: The Two-Week Wait and Pregnancy Confirmation
Following the insemination, the Intrauterine Insemination Process enters its final and often most emotionally challenging phase: the “two-week wait” (TWW) and the eventual pregnancy test. This period is marked by anticipation, patience, and careful monitoring for any post-IUI instructions.
Post-IUI Instructions and Supporting Medications
After the IUI procedure, your fertility specialist may provide specific instructions to support your body during the implantation window. It’s common for some women to be prescribed progesterone after IUI. This hormone helps to thicken and support the uterine lining, creating an optimal environment for a fertilized egg to implant and grow.
You’ll be advised on how to administer these medications, typically orally or vaginally. Beyond medication, general advice often includes maintaining a healthy lifestyle, avoiding overly strenuous activities for a few days, and refraining from internal bathing or tampons. The goal is to create the best possible conditions within your body for a potential pregnancy. https://dorengynaecareivffertility.com/in-vitro-fertilization-ivf/
Managing the “Two-Week Wait” (TWW)
The “two-week wait” is precisely what it sounds like: the period between the IUI procedure and the date of your official pregnancy test. This phase can be emotionally intense, filled with a mix of hope, anxiety, and constant self-analysis for any early pregnancy symptoms. It’s crucial during this time to practice stress management techniques.
Engaging in calming activities like light walks, meditation, or spending time with supportive loved ones can be beneficial. It’s also important to resist the urge to take at-home pregnancy tests too early. These tests may not be sensitive enough to detect pregnancy hormones in the initial days after implantation, leading to false negative results and unnecessary emotional distress. Trust your clinic’s timeline for the official test.
Official Pregnancy Test and Next Steps
Approximately 10 to 14 days after your IUI, your fertility clinic will schedule an official pregnancy test, usually a blood test. A blood test is more sensitive and provides a definitive answer compared to urine tests. A positive result confirms pregnancy, and your clinic will then guide you on the next steps, which typically involve scheduling an early pregnancy scan to confirm the location and viability of the pregnancy.
If the result is negative, it’s natural to feel disappointed. Your specialist will discuss what happens next, whether it involves reviewing your IUI success rates for previous cycles, considering another Intrauterine Insemination Process cycle, or exploring alternative fertility treatment options such as IUI vs. IVF, to determine the best path forward for your family-building journey.
Conclusion:
Navigating Your Intrauterine Insemination Process with Confidence
The Intrauterine Insemination Process is a well-established and effective pathway for many seeking to expand their families. By understanding its four distinct phases—initial assessment, ovarian stimulation, sperm preparation and insemination, and the two-week wait—you gain valuable insight into what to expect at each step.
While the journey can be challenging, knowing the process empowers you to participate actively in your care. Remember, successful IUI treatment hinges on meticulous planning, precise timing, and professional guidance. We encourage you to maintain open communication with your reproductive specialist. They are your best resource for personalized advice, ensuring you navigate your IUI journey with confidence, hope, and the best possible chances of achieving your fertility goals.
Is the Intrauterine Insemination (IUI) Procedure Painful?
Most women report mild discomfort during the IUI procedure, often comparing it to a routine Pap smear. Anesthesia is not typically required. While some women may experience light cramping or spotting afterward, this is generally normal and subsides quickly.
What is the Success Rate for Intrauterine Insemination?
IUI success rates vary depending on numerous factors, including the individual’s age, the specific cause of infertility, and whether fertility medications are used. On average, success rates per cycle typically range from 10-20%. It’s important to note that cumulative success rates often increase with multiple cycles. Your fertility specialist can provide more specific data based on your unique profile.
How Many IUI Cycles are Recommended Before Considering IVF?
The number of recommended IUI cycles before considering IVF often depends on individual circumstances, including age and diagnosis. For women under 35 with unexplained infertility, for instance, 3 to 6 cycles may be suggested. For those over 35 or with specific diagnoses, typically 3 cycles are recommended before exploring other fertility treatment options like IVF, which often offers higher success rates in certain situations. Your specialist will guide this decision.
How Much Does the Intrauterine Insemination Process Cost?
The IUI cost can vary significantly depending on factors such as your insurance coverage in Lekki, Lagos, Nigeria, the specific clinic you attend, and whether fertility medications are needed (as these can add substantially to the total). Without insurance, a single Intrauterine Insemination Process cycle can range from a few hundred to over a thousand dollars (USD equivalent), but it’s essential to get a direct quote from your chosen clinic for local pricing.